Medical Claims Assessor
Eastwest Healthcare Inc.
وصف الوظيفة
Key Responsibilities:
Claims Processing – Timeliness and Accuracy
- Review and process medical claims within the standard processing time.
- Ensure accuracy of approved amounts, encoding, and benefits of coverage in line with policies and member entitlements.
Daily Productivity Management
- Meet or exceed daily claims processing targets while maintaining high standards of accuracy and quality.
- Organize workload to ensure consistent processing volume and timely completion.
Compliance and Quality Assurance
- Ensure all processed claims comply with internal policies, medical necessity guidelines, and benefit limitations.
- Flag and escalate discrepancies, incomplete documents, or non-compliant claims for further review.
Data Entry and System Updates
- Accurately encode claims information into the processing system.
- Update claim statuses and resolution notes as required.
Internal Coordination
- Coordinate with internal department to clarify claim issues, seek approvals, or complete documentation.
- Provide support in resolving inquiries related to processed claims.
Continuous Improvement
- Recommend ideas for workflow improvement to reduce bottlenecks and increase efficiency.
- Participate in trainings and calibration sessions to stay updated with policy changes and system updates.
JOB QUALIFICATIONS:
Educational Attainment
- Bachelor's degree in Nursing, Allied Health, Business Administration, or any related field
- Associate degree holders with relevant experience may also be considered
Relevant Experience
- At least 1-2 years of experience in medical claims processing, health insurance operations, or related administrative/ healthcare roles
Areas of Experience
- Medical claims review and processing
- Health insurance or HMO operations
- Data entry and documentation
- Coordination with customers or internal stakeholders
Knowledge
- Basic understanding of medical terms, procedures, and diagnosis codes
- Knowledge of health insurance policies, benefits and claims guidelines
- Familiarity with medical necessity standards and benefit limits
- Proficiency in claims processing system and MS Office applications
Skills
- Strong analytical and decision- making skills
- High attention to detail and accuracy
- Good time management or organization skills
- Clear written and verbal communication
- Fast and accurate data entry skills
- Ability to stay focus during repetitive tasks
Competencies
- Commitment to compliance and quality
- Productivity and results- driven mindset
- Problem- solving and critical thinking
- Integrity and confidentiality
- Teamwork and collaboration
- Adaptability to changing processes
Licensure
- Not Required
- Nursing or medical-related licensure/certification is an advantage
Other Requirements
- Willing to work onsite and on shifting schedules
- Comfortable working with quotas, deadlines, and a fast-paced environment
- Open to training and continuous learning
Job Type: Full-time
Work Location: In person
Edlyn Sanchez
HR OfficerEastwest Healthcare Inc.
أكثر من عشرة ردود اليوم
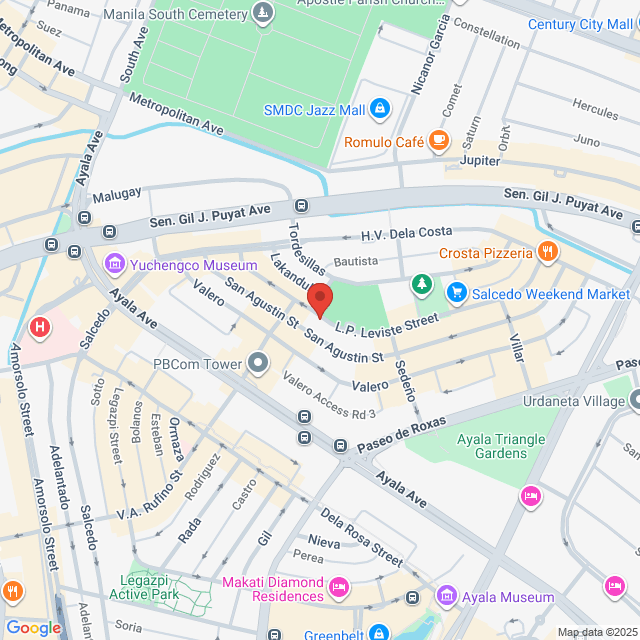
موقع العمل
6/F Makati Executive Center, V.A Rufino St., cor L.P Leviste St., Salcedo Village, Makati City, Salcedo Village Makati city
نشر بتاريخ 20 November 2025
استكشاف وظائف مماثلة
عرض المزيد من الوظائف المشابهةClaims Support Role
 Mesco Express Service Corporation
Mesco Express Service Corporation1.6-1.8Kر.س[شهريًا]
في الموقع - ماكاتي<1 سنة خبرةبكالوريوسدوام كامل

Nanan DiñoVice President
Claims Supervisor
 Manila Bankers Life and General Assurance Corporation
Manila Bankers Life and General Assurance Corporation1.9-2.6Kر.س[شهريًا]
في الموقع - ماكاتي3-5 سنوات خبرةبكالوريوسدوام كامل

Recruitment opgOwner
Claims Processor
 Paramount Life & General Insurance Corporation
Paramount Life & General Insurance Corporation1.3-1.6Kر.س[شهريًا]
في الموقع - ماكاتي1-3 سنوات خبرةبكالوريوسدوام كامل

renee.ursua hrRecruiter
Claims Specialist
 SPD Jobs Incorporated
SPD Jobs Incorporated1.2-1.3Kر.س[شهريًا]
في الموقع - ماكاتيخريج جديد/طالببكالوريوسدوام كامل

Jannelle SombrioRecruitment Supervisor
Claims Specialist
 BPI MS Insurance Corporation
BPI MS Insurance Corporation956-1.3Kر.س[شهريًا]
في الموقع - ماكاتي1-3 سنوات خبرةبكالوريوسدوام كامل

Andres Irad CasidsidHR Manager

Eastwest Healthcare Inc.
<50 موظف
التأمين والمعاشات
View jobs hiring
سجل للدردشة مع المدير
تذكير أمان Bossjob
إذا كانت الوظيفة تتطلب العمل خارج البلاد، يرجى أن تكون متيقظًا وأن تحذر من الاحتيال.
إذا واجهت صاحب عمل قام بالإجراءات التالية أثناء بحثك عن وظيفة، يرجى الإبلاغ عنه فورًا
- يحجب هويتك،
- يتطلب منك تقديم ضمان أو يجمع ممتلكات،
- يجبرك على الاستثمار أو جمع الأموال،
- يجمع فوائد غير قانونية،
- أو حالات غير قانونية أخرى.